NHSA Insurance Funding Expert Zheng Jie: Shifting from Excessive Price Reduction to Value-Based Procurement for China's Drug Pricing Dilemma

At the 5th China Rare Disease Cooperation and Exchange Conference, Zheng Jie, the leader of the Insurance Funding Analysis Expert Group for the 2020, 2021, and 2022 NRDL negotiations, addressed the question of how China's national negotiation can tackle the challenge of access to rare disease drugs. Zheng Jie proposed a comprehensive overhaul of the drug value system to achieve precise pharmaceutical pricing.
Key points from Zheng Jie's presentation:
- Advocating a shift from excessive price reduction strategies.
- Emphasizing the transition from a bottom-fishing pricing approach to value-based procurement based on drug classification.
- Laying the groundwork for more favorable policy support for high-value innovative therapies to be included in China's national reimbursement drug listing.
Below is a summary of his presentation.
Downsides of Excessive Price Reduction
Reducing prices without thoughtful consideration is not sustainable.
- First, Excessive price cuts hinder R&D efforts of innovative pharma firms, especially for high-value therapies like rare disease drugs.
- Second, it is prone to breed issues such as quality risks and cutthroat competition.
Revamping the Entire Drug Value System
- First, Transition from bottom-fishing pricing to value-driven procurement by understanding the medical insurance fund's budget.
- Second, reconstruct the value system, use objective methods for accurate drug value assessment, and align drug prices with their true value.
Create a Well-Structured Medical Insurance Fund Budget Model
- Include fund budget, policy, and model factors in building the budget model.
- Establish annual allocations for drug expenses, specific drug policies, and various therapeutic categories.
- If funding for a specific therapy area is excessive, it can be reduced and redirected to areas like rare diseases in need of policy support.
Revamping the Value System: Ensuring Accurate Pharmaceutical Pricing
- Employ a tiered evaluation system.
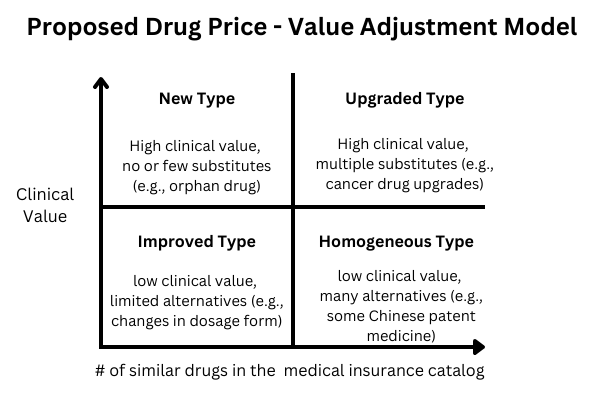
- Classify drugs based on clinical expert evaluations (Y-axis) and the number of similar drugs available in the medical insurance catalog (X-axis).
- Allocate resources and budgets based on drug classifications for accurate pharmaceutical pricing.
- New Type: These drugs are of high clinical value and have no or few substitutes within the insurance catalog. Examples include orphan drugs. Encourage inclusion, preferential policies, and increased support.
- Upgraded Type: These drugs possess high clinical value but face competition from multiple substitutes within the catalog. This is frequently observed in the context of cancer drug upgrades or replacements. Encourage inclusion and provide more support.
- Improved Type: Drugs in this category may not have high clinical value, but they have limited alternatives within the catalog. This often involves changes in dosage forms serving specific populations. Encourages inclusion and suggests achieving higher cost-effectiveness.
- Homogeneous Type: These drugs receive low clinical ratings and have numerous similar alternatives in the catalog—inclusion based on achieving higher cost-effectiveness.
2021 NRDL Negotiation Results
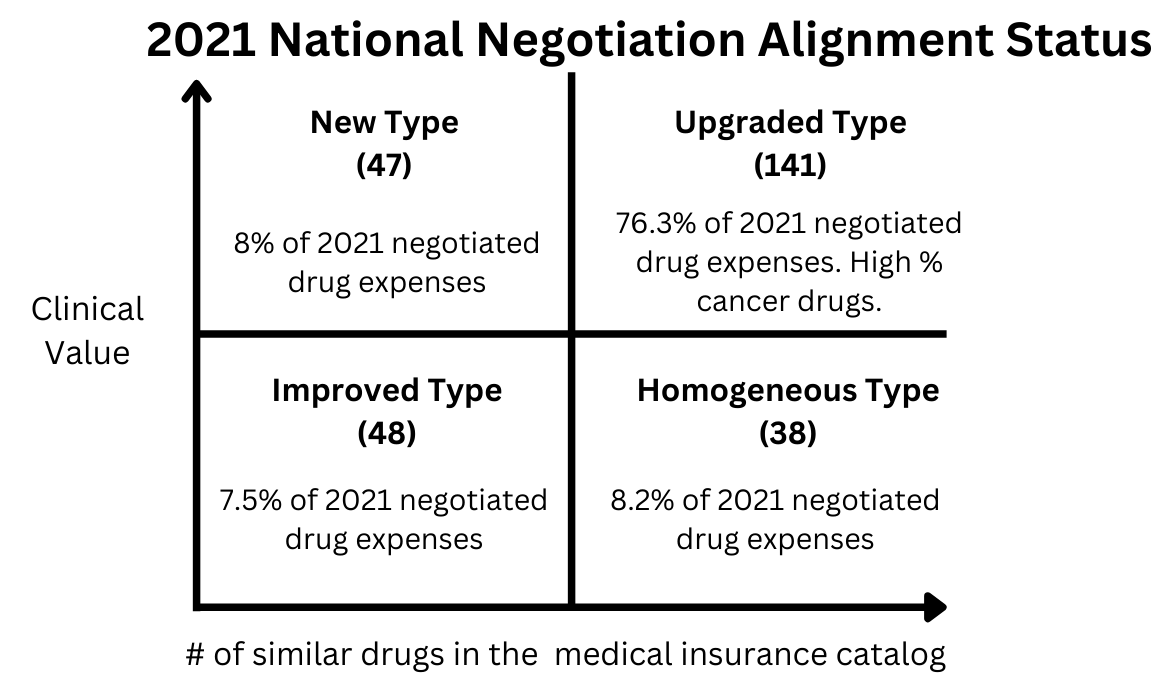
Applying this model to analyze several years of 'national drug negotiations' yields the following results: "new type” accounting for just 8% of negotiated drug expenses in 2021. This suggests that policies can confidently endorse and support this category without concerns about depleting medical insurance resources.
Moving Forward
The preceding information presents theories and methods developed by the National Drug Negotiation Insurance Funding Analysis Expert Group over the years.
In the future, it's crucial to use this model to transition national drug negotiations from bottom-fishing pricing to a fair allocation of medical insurance resources. This aligns with efforts to restructure the pharmaceutical value system to restore market values, channel resources toward valuable medications, and advance pharmaceutical innovation.
Reform is incremental, and there may not be immediate solutions to meet all demands. Progressing from a state without methods to achieving scientific rationality is a step-by-step journey we collectively aspire to.
References:
- 郑杰:围绕医保基金可支配空间,重构全药物价值体系, 健康界, 2023-09-07, https://new.qq.com/rain/a/20230907A0AQN300





